NEWSROOM
NEWSROOM
Understanding Diabetes Medications: A Guide for Type 2 Diabetes
Understanding Diabetes Medications: A Guide for Type 2 Diabetes
Understanding Diabetes Medications: A Guide for Type 2 Diabetes
By:
Dr. Samuel Lim
Thursday, January 8, 2026
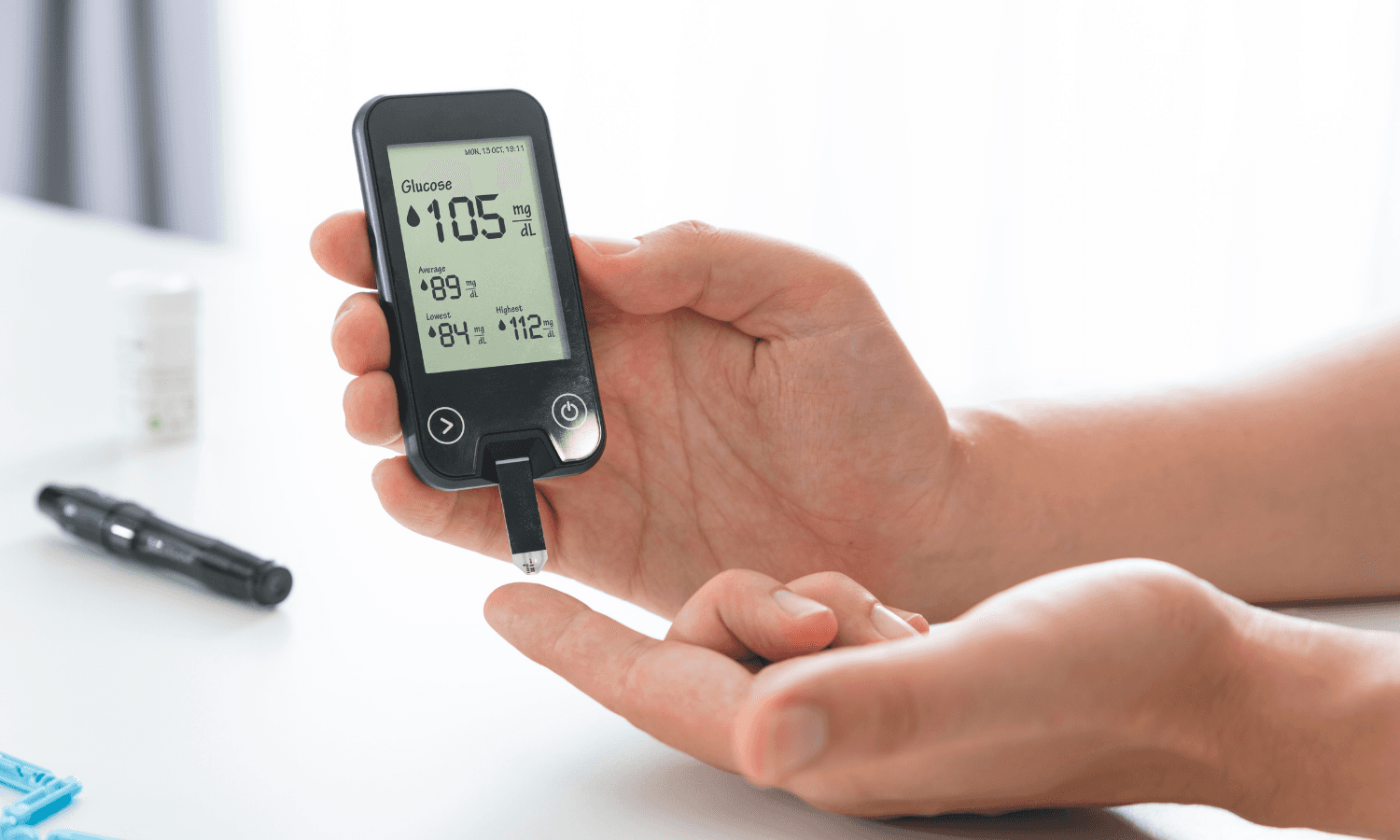
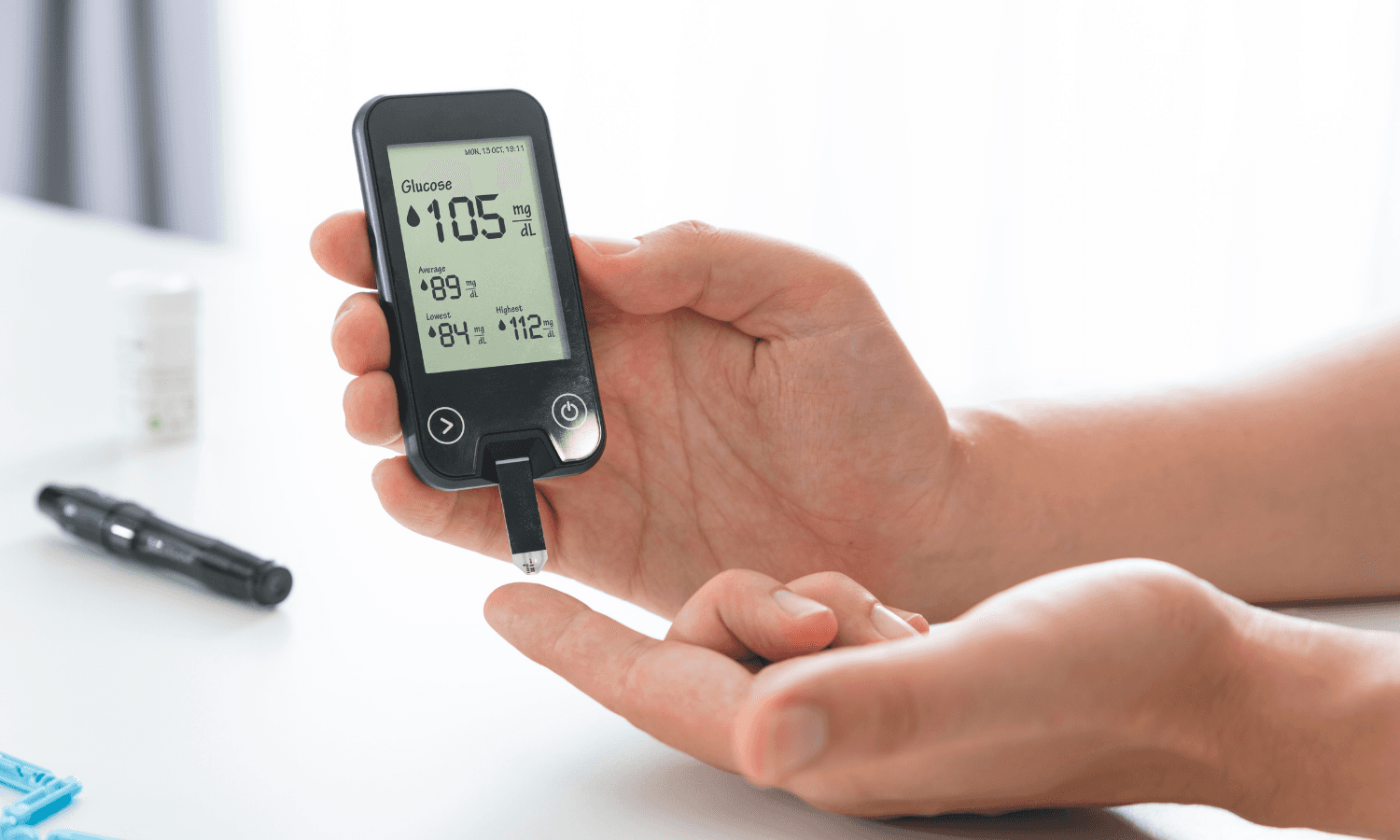
Type 2 diabetes mellitus is a common long-term condition where blood sugar levels remain higher than normal. When left uncontrolled, diabetes can quietly damage the heart, kidneys, eyes, nerves, and blood vessels over time.
Lifestyle measures such as diet, weight management, and regular exercise form the foundation of diabetes care. However, many patients will also require medications to keep blood sugar within a healthy range and reduce the risk of long-term complications.
Why Diabetes Medications Are Important
Type 2 diabetes is a progressive condition. Even with good lifestyle habits, the body may gradually become less effective at controlling blood sugar. Medications help support this process by improving insulin action, reducing sugar production, or increasing sugar excretion.
The goal of treatment is not just to lower blood sugar numbers, but to protect long-term health and maintain quality of life.
Common Types of Diabetes Medications
There is no single “best” diabetes medication for everyone. Treatment is individualised based on blood sugar levels, weight, kidney and heart health, risk of low blood sugar, cost, and daily routine.
Below are some of the most commonly used medications in Type 2 diabetes.
Metformin
Metformin is usually the first medication prescribed for Type 2 diabetes. It works by reducing glucose production by the liver and improving the body’s sensitivity to insulin.
It is effective, well-studied, and has a very low risk of causing low blood sugar. Importantly, it does not cause weight gain.
Some patients may experience stomach-related side effects such as bloating, nausea, or diarrhoea, especially when starting treatment. Taking the medication with meals or using the extended-release formulation often improves tolerability.
Sulfonylureas
Sulfonylureas help lower blood sugar by stimulating the pancreas to release more insulin. They are commonly added when blood sugar remains high despite metformin therapy.
Common examples include:
Glipizide
Gliclazide
While effective, these medications can cause low blood sugar, particularly if meals are delayed or skipped, and may lead to weight gain. Patients should be familiar with symptoms of hypoglycaemia, such as sweating, shakiness, or dizziness.
DPP-4 Inhibitors
DPP-4 inhibitors work by increasing natural gut hormones that enhance insulin release after meals and reduce glucose production by the liver.
Common examples include:
Sitagliptin
Linagliptin
These medications are generally well tolerated, weight neutral, and carry a very low risk of hypoglycaemia. Linagliptin is especially convenient for patients with kidney disease, as dose adjustment is not required.
SGLT2 Inhibitors
SGLT2 inhibitors lower blood sugar by allowing excess glucose to be excreted through the urine.
Common examples include:
Empagliflozin
Dapagliflozin
Canagliflozin
In addition to blood sugar control, this class offers benefits such as weight loss, blood pressure reduction, and protection for the heart and kidneys. Possible side effects include increased urination and a higher risk of genital or urinary tract infections. Good hydration and hygiene can help reduce these risks.
Injectable Therapies
Injectable medications are considered when oral medications are insufficient.
GLP-1 receptor agonists, such as Liraglutide and Semaglutide, improve insulin release after meals, reduce appetite, promote weight loss, and provide cardiovascular benefits. These are typically given once daily or once weekly.
Insulin therapy is required when other treatments can no longer maintain blood sugar targets. Starting insulin is not a failure — it reflects the natural progression of diabetes and is an effective way to protect long-term health.
Individualised Treatment Is Key
Many patients require a combination of medications to achieve good control. Doctors tailor treatment plans based on:
Blood sugar trends
Body weight
Kidney and heart health
Risk of low blood sugar
Cost and convenience
Managing Diabetes for the Long Term
Good diabetes care goes beyond medication alone. The aim is to reduce complications, preserve organ function, and support a good quality of life.
If you have questions about your diabetes medications, side effects, or treatment plan, we encourage you to speak with us.
Book a teleconsult or clinic appointment to review your diabetes management and optimise your long-term health.
Type 2 diabetes mellitus is a common long-term condition where blood sugar levels remain higher than normal. When left uncontrolled, diabetes can quietly damage the heart, kidneys, eyes, nerves, and blood vessels over time.
Lifestyle measures such as diet, weight management, and regular exercise form the foundation of diabetes care. However, many patients will also require medications to keep blood sugar within a healthy range and reduce the risk of long-term complications.
Why Diabetes Medications Are Important
Type 2 diabetes is a progressive condition. Even with good lifestyle habits, the body may gradually become less effective at controlling blood sugar. Medications help support this process by improving insulin action, reducing sugar production, or increasing sugar excretion.
The goal of treatment is not just to lower blood sugar numbers, but to protect long-term health and maintain quality of life.
Common Types of Diabetes Medications
There is no single “best” diabetes medication for everyone. Treatment is individualised based on blood sugar levels, weight, kidney and heart health, risk of low blood sugar, cost, and daily routine.
Below are some of the most commonly used medications in Type 2 diabetes.
Metformin
Metformin is usually the first medication prescribed for Type 2 diabetes. It works by reducing glucose production by the liver and improving the body’s sensitivity to insulin.
It is effective, well-studied, and has a very low risk of causing low blood sugar. Importantly, it does not cause weight gain.
Some patients may experience stomach-related side effects such as bloating, nausea, or diarrhoea, especially when starting treatment. Taking the medication with meals or using the extended-release formulation often improves tolerability.
Sulfonylureas
Sulfonylureas help lower blood sugar by stimulating the pancreas to release more insulin. They are commonly added when blood sugar remains high despite metformin therapy.
Common examples include:
Glipizide
Gliclazide
While effective, these medications can cause low blood sugar, particularly if meals are delayed or skipped, and may lead to weight gain. Patients should be familiar with symptoms of hypoglycaemia, such as sweating, shakiness, or dizziness.
DPP-4 Inhibitors
DPP-4 inhibitors work by increasing natural gut hormones that enhance insulin release after meals and reduce glucose production by the liver.
Common examples include:
Sitagliptin
Linagliptin
These medications are generally well tolerated, weight neutral, and carry a very low risk of hypoglycaemia. Linagliptin is especially convenient for patients with kidney disease, as dose adjustment is not required.
SGLT2 Inhibitors
SGLT2 inhibitors lower blood sugar by allowing excess glucose to be excreted through the urine.
Common examples include:
Empagliflozin
Dapagliflozin
Canagliflozin
In addition to blood sugar control, this class offers benefits such as weight loss, blood pressure reduction, and protection for the heart and kidneys. Possible side effects include increased urination and a higher risk of genital or urinary tract infections. Good hydration and hygiene can help reduce these risks.
Injectable Therapies
Injectable medications are considered when oral medications are insufficient.
GLP-1 receptor agonists, such as Liraglutide and Semaglutide, improve insulin release after meals, reduce appetite, promote weight loss, and provide cardiovascular benefits. These are typically given once daily or once weekly.
Insulin therapy is required when other treatments can no longer maintain blood sugar targets. Starting insulin is not a failure — it reflects the natural progression of diabetes and is an effective way to protect long-term health.
Individualised Treatment Is Key
Many patients require a combination of medications to achieve good control. Doctors tailor treatment plans based on:
Blood sugar trends
Body weight
Kidney and heart health
Risk of low blood sugar
Cost and convenience
Managing Diabetes for the Long Term
Good diabetes care goes beyond medication alone. The aim is to reduce complications, preserve organ function, and support a good quality of life.
If you have questions about your diabetes medications, side effects, or treatment plan, we encourage you to speak with us.
Book a teleconsult or clinic appointment to review your diabetes management and optimise your long-term health.
Book Appointment


OUR NEWS
OUR NEWS
Latest News & Articles
Latest News & Articles
Latest News & Articles

Rei Huan
Thursday, February 26, 2026

Rei Huan
Thursday, February 26, 2026

Rei Huan
Friday, February 6, 2026

Rei Huan
Friday, February 6, 2026

Dr. Samuel Lim
Sunday, February 1, 2026

Dr. Samuel Lim
Sunday, February 1, 2026

Rei Huan
Thursday, February 26, 2026

Rei Huan
Friday, February 6, 2026
